Combining a Cleaned-Out Pig Heart with a Patient’s Own Stem Cells
Heart disease is the leading cause of death worldwide. The World Health Organization estimates that 17.9 million people lose their lives to it each year, accounting for 32% of global deaths.
Doris Taylor is a scientist working in regenerative medicine and tissue engineering. Her work has focused on creating personalized functioning human hearts in a lab that could rule out the need for donors. Taylor has dubbed these hearts “ghost hearts.” This article was republished with permission from The Conversation, a news site dedicated to sharing ideas from academic experts like Doris Taylor, Regenerative Medicine Lecturer at the University of New Hampshire.
What are the biggest challenges facing organ donations today?
Currently, patients in need of a heart transplant need to join a waitlist, and hearts become available when someone else has died. Because there are not enough hearts to go around, only the very sick are put on the waitlist. The U.S. transplants about 11 hearts a day, and on a given day there are more than 3,000 people waiting for a heart.
Even when organs are successfully transplanted, it isn’t a Hollywood fairy-tale ending. A person receiving an organ transplant essentially trades one disease for other medical complications and diseases. Toxic drugs necessary to prevent rejection can cause high blood pressure diabetes, cancer and kidney failure. These are serious medical issues that also affect people emotionally, financially and physically.
About 18% of people die in the first year after a transplant.
What is the so-called “ghost heart”? How does it work?
The ghost heart is a heart whose cells have been removed. All that remains is the heart framework, or scaffolding. It’s called a ghost heart because removing the cells causes the heart to turn from red to white. A human heart wouldn’t work as a scaffold because so few are available to work with.
So my team and I went with the next best thing: a pig heart. Pig hearts are similar to human hearts in terms of their size and structure. Both have four chambers – two atria and two ventricles – responsible for pumping blood. And structures from pig hearts such as valves have been used in humans safely.
To remove the cells, the pig heart is gently washed through its blood vessels with a mild detergent to remove the cells. This process is called perfusion decellurization. The cell-free heart can then be seeded with new cells – in this case, a patient’s cells – thus forming a personalized heart.
What role do stem cells play in creating a heart?
If you lined up the cells needed for an average-size 350-gram human heart, they would stretch for 41,000 miles. Stacked on top of one another, they would amount to 2 billion lines of cells, or enough to fill seven movie screens. But heart cells don’t divide. If they did, hearts could likely repair themselves.
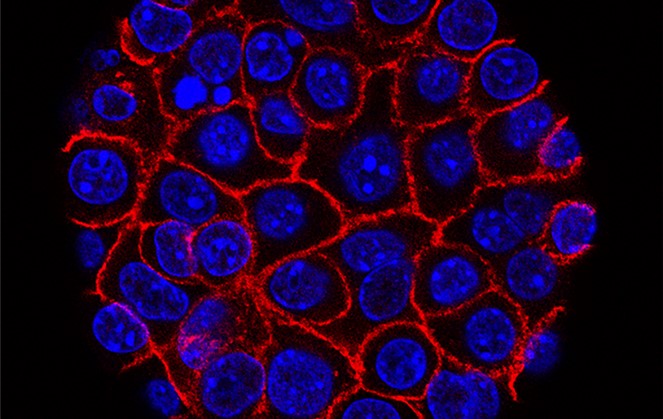
Stem cells, on the other hand, do divide. They can also form into specialized cells – in this case, heart cells. Nobel Prize laureate Dr. Shinya Yamanaka discovered a method to make stem cells out of blood or skin cells from an adult. My team and I employed this method to obtain stem cells, then grew those cells into billions. After that, the team used chemicals to “differentiate” them into heart cells. We employed this method to obtain billions and billions of heart cells.
The first time I saw heart cells beating in a dish it was life-changing. But while the cells are alive and beat, they are not a heart. To be a heart, these cells need to be placed into a form that lets them become a unified organ, to mature and to be able to pump blood. In a human body, this happens during development; we had to reproduce that capacity in the lab.
In 2022, a pig heart that had been genetically engineered to reduce rejection and improve acceptance was transplanted into a human. Why is it better to build a heart from scratch using pig scaffolding instead?
Let me be clear: Any heart is better than no heart. And xenotransplantation – the process by which nonhuman animal organs are transplanted into humans – opened doors for all scientists in this field.
The patient received a pig heart that had been gene-edited. Human genes were added, and some pig genes were removed, but the heart still essentially comprised pig cells within a pig scaffold. As a result, the individual had to take anti-rejection drugs that suppressed the immune system. And, unbeknownst to doctors, the heart was carrying a pig virus that ultimately killed the patient two months following the transplant.
I believe these sorts of problems are avoided with the ghost heart. My team removes the pig cellular material from the scaffold, leaving only the protein structure and blood vessel channels behind. The proteins are so similar to human scaffold proteins they don’t appear to cause rejection.