Fragile X Syndrome Often Results from Improperly Processed Genetic Material – Correctly Cutting RNA Offers a Potential Treatment
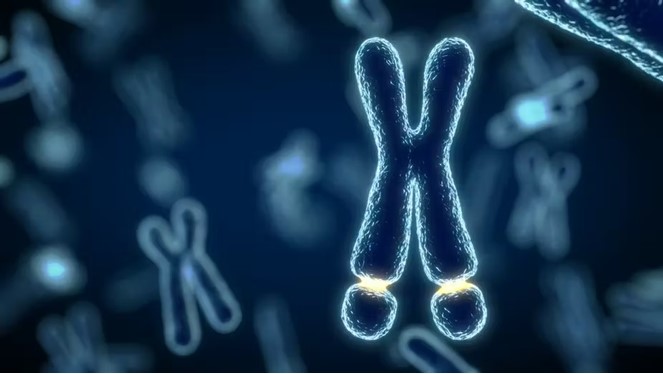
Fragile X syndrome is a genetic disorder caused by a mutation in a gene that lies at the tip of the X chromosome. It is linked to autism spectrum disorders. People with fragile X experience a range of symptoms that include cognitive impairment, developmental and speech delays and hyperactivity. They may also have some physical features such as large ears and foreheads, flabby muscles and poor coordination.
This article was republished with permission from The Conversation, a news site dedicated to sharing ideas from academic experts. It represents the research-based findings and thoughts of, Joel Richter, Professor of Neuroscience, UMass Chan Medical School and Sneha Shah, Assistant Professor of Molecular Medicine. UMass Chan Medical School
Along with our colleagues Jonathan Watts and Elizabeth Berry-Kravis, we are a team of scientists with expertise in molecular biology, nucleic acid chemistry and pediatric neurology. We recently discovered that the mutated gene responsible for fragile X syndrome is active in most people with the disorder, not silenced as previously thought. But the affected gene on the X chromosome is still unable to produce the protein it codes for because the genetic material isn’t properly processed. Correcting this processing error suggests that a potential treatment for symptoms of fragile X may one day be available.
Repairing Faulty RNA Splicing
The FMR1 gene encodes a protein that regulates protein synthesis. A lack of this protein leads to overall excessive protein synthesis in the brain that results in many of the symptoms of fragile X.
The mutation that causes fragile X results in extra copies of a DNA sequence called a CGG repeat. Everyone has CGG repeats in their FMR1 gene, but typically fewer than 55 copies. Having 200 or more CGG repeats silences the FMR1 gene and results in fragile X syndrome. However, we found that around 70% of people with fragile X still have an active FMR1 gene their cellular machinery can read. But it is mutated enough that it is unable to direct the cell to produce the protein it encodes.
Genes are transcribed into another form of genetic material called RNA that cells use to make proteins. Normally, genes are processed before transcription in order to make a readable strand of RNA. This involves removing the noncoding sequences that interrupt genes and splicing the genetic material back together. For people with fragile X, the cellular machinery that does this cutting incorrectly splices the genetic material, such that the protein the FMR1 gene codes for is not produced.
Fragile X syndrome is the most common inherited form of intellectual disability.
Using cell cultures in the lab, we found that correcting this missplice can restore proper RNA function and produce the FMR1 gene’s protein. We did this by using short bits of DNA called antisense oligonucleotides, or ASOs. When these bits of genetic material bind to RNA molecules, they change the way the cell can read it. That can have effects on which proteins the cell can successfully produce.
ASOs have been used with spectacular success to treat other childhood disorders, such as spinal muscular atrophy, and are now being used to treat a variety of neurological diseases.
Beyond Mice Models
Notably, fragile X syndrome is most often studied using mouse models. However, because these mice have been genetically engineered to lack a functional FMR1 gene, they are quite different from people with fragile X. In people, it is not a missing gene that causes fragile X but mutations that lead the existing gene to lose function.
Because the mouse model of fragile X lacks the FMR1 gene, the RNA is not made and so cannot be misspliced. Our discovery would not have been possible if we used mice.
With further research, future studies in people may one day include injecting ASOs into the cerebrospinal fluid of fragile X patients, where it will travel to the brain and hopefully restore proper function of the FMR1 gene and improve their cognitive function.